cancer
Will doctors use AI-powered oncology tools?
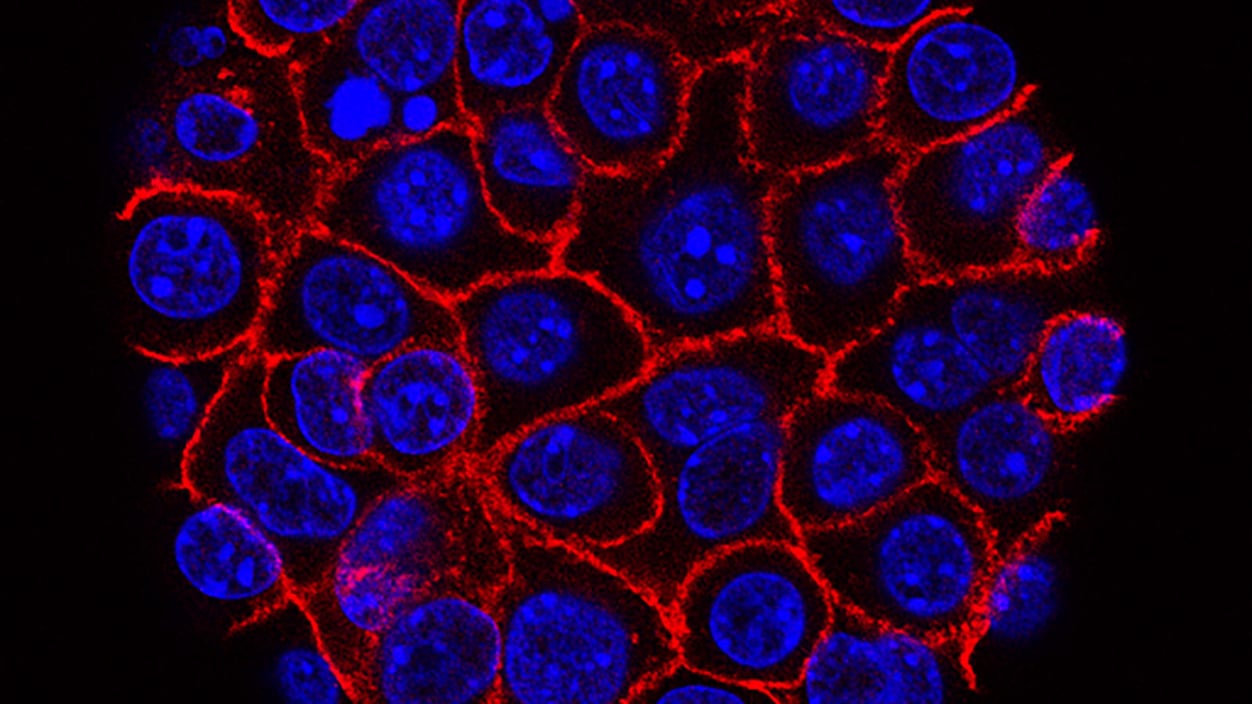
National Cancer Institute/USC Norris Comprehensive Cancer Center
Here’s a moment in the practice of medicine that experts agree could be eased by AI: when an oncologist doesn’t have a clear indication which treatment will work better for a patient. Each unsuccessful treatment takes, and wastes, precious time. To address this issue, companies are developing AI-powered digital pathology tools that can glean more information about a tumor than a doctor’s human eyes can see.
“I think it’s a really promising direction for getting the right treatment to the right person,” oncologist Danielle Bitterman said. But how comfortable doctors feel actually using these tools will depend on many factors, including the strength of the clinical validation and the transparency of the algorithm. Read more from STAT’s Angus Chen on what tools have already hit the market and the data backing them up.
notable quotable
‘In general, we’ve been very pro vaccines … Now, you can never make everybody happy’
That was FDA Commissioner Marty Makary speaking yesterday at an event held by the pharmaceutical industry group PhRMA. Makary struck a decidedly different tone than the other top federal health official at the forum, CMS Administrator Mehmet Oz. Oz had a friendly on-stage conversation with Pfizer CEO and PhRMA board chair Albert Bourla in which he talked about the benefits of vaccines, welcomed the idea of closed-door meetings with executives, and suggested industry leaders consider government jobs.
But Makary was grilled by former CNBC reporter Bertha Coombs about the agency’s more skeptical approach to the regulation of vaccines, including the recent decision by top official Vinay Prasad to refuse to review Moderna’s application for a new flu shot. Read more from STAT’s Lizzy Lawrence and Daniel Payne about the industry’s seemingly positive relationship with Oz and its more tenuous feelings toward Makary.
first opinion
Same blood test, different results
In the midst of a health crisis a few years ago, patient advocate Samantha Bonsack learned a startling fact: The thyroid-stimulating hormone test — one of the most commonly ordered laboratory blood tests in the country — is not standardized. Depending on which company’s analyzer processes the blood, the same sample can yield results differing from 20% to 40%.
“What makes this failure especially frustrating is that the scientific solution already exists,” Bonsack writes in a new First Opinion essay. The CDC, along with an international clinical chemistry group, created a validated protocol to streamline the results from different companies. But the FDA has never required manufacturers to recalibrate, and the CDC lacks enforcement power. Read more on what Bonsack says should be a straightforward fix to this long-ignored problem.
